Gastric Band Removal in Dubai
If you had a gastric band but have not lost weight or have problems with a band like vomiting, restrictions, or if you have developed complications like a slippage/erosion or are simply considering Gastric band removal in Dubai, please contact Dr. Girish Juneja.
Gastric (Stomach) Restrictive Procedures Gastric Banding, Dubai
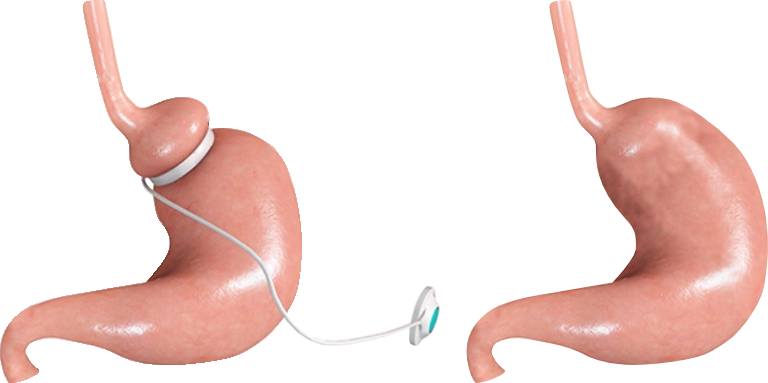
Laparoscopic gastric banding is another restrictive gastric approach taken for weight loss surgery in Dubai. This procedure, which was approved in the U.S. in June 2001, is popular since it is “high tech” (utilizes a laparoscope, an instrument which is inserted into the abdominal cavity), and recovery time is only a few days. Basically, an adjustable band is placed around the upper portion of the stomach, resulting in (essentially) a much smaller stomach. This restricts the amount of food that can be eaten, similar to the vertical banded gastroplasty (see above).

Why Gastric band removal ?
In long term, gastric band patients develop acid reflux, vomiting, tightness in chest ,dysphagia, slippage beside regaining weight . If you have developed any of these problems post gastric band surgery then you should have a thorough & urgent checkup about your band as these problems may be an indication of developing risky & life threatening complications & if so then urgent removal is needed. Otherwise also you should have periodic checkup to catch these problems early.
How it is done ?
Gastric band removal in Dubai is done laparoscopically means surgically. You have to stay one day in hospital and recovery is very fast.


